Plantar Fasciitis, or more commonly known as: When you wake up in the morning and it feels like someone was stabbing you in the bottom of your foot all night.
If that describes you, here are a couple more questions:
Does it hurt even more the day after you run?
Does it make running all but impossible or even more unbearable than it already is? #runningsucks
If so, you’re one of a few million people learning about Plantar Fasciitis the hard way and I want to help you fix that so you can get back to pain free training.
There are a couple very common running injuries that, sadly, many runners just chalk up as part of the process even though they are entirely preventable with proper training (and attention to movement).
Plantar Fasciitis is one of the most painful because it seems to stick around long after you’re done training.
So, let’s talk about Plantar Fasciitis.
As one of the most common causes of heel pain (I’d say of foot/heel pain in general) Plantar Fasciitis is something I know a ton of you guys/gals are dealing with or have dealt with in the past. And it’s no fun.
So first, let’s knock out some basic definitions so you have a better understanding of what I’m talking about.
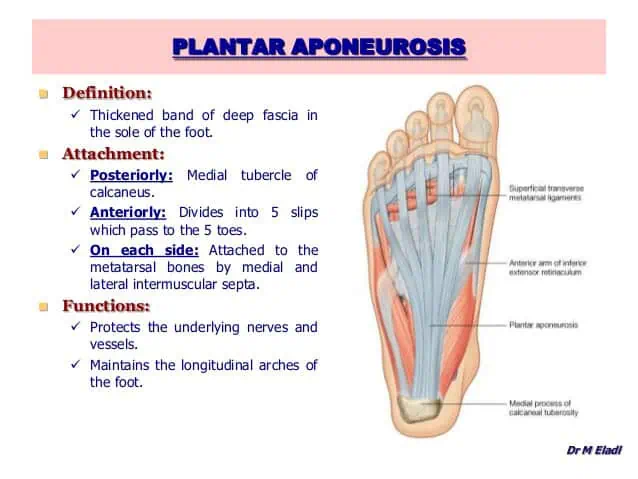
Plantar Fasciitis is caused by swelling and inflammation of the Plantar Aponeurosis (Fascia) and it manifests as a sharp, stabbing pain in the bottom of your foot and/or heel.
And it’s typically worse in the morning when you wake up.
So basically, when the soft tissues surrounding your foot, heel, and ankle get angry they tighten up (Way more than a sore muscle) and cause all kinds of fun pain.
The good news is that once you get those tissues warmed up and moving the pain typically subsides a bit.
The bad news is that unless you treat the root cause of the problem the pain will come back and you’ll be dealing with issues for a while.
Quick Disclaimer: I’m not a doctor & I don’t play one of TV. This article is for educational purposes only and if you DO have an injury or problem go seek competent medical advice (If you can find it!)
Who gets Plantar Fasciitis?
Plantar Fasciitis is super common in a few different populations.
First, people who run a lot are typically at the highest risk because of the stress and strain put on the feet while running.
If you think about the force being absorbed by each foot as you run (>2.5x Bodyweight) and you consider this is happening at a rate of around 330 times per 400m (1/4 mile) then you can see that the stress can add up super fast.
Second, if you ruck a lot then you may have dealt with this as well. With the added weight of the ruck combined with the heel to toe motion of walking/rucking your feet take a lot of punishment.
Third, if you’ve recently jumped on the minimalist shoe train (you should if you haven’t, at least in your training) you may have noticed a significant increase in foot, ankle, and calf stress / soreness.
This is exactly why I suggest people transition into a more minimal shoe over the course of months and not days. You body will adapt but it takes time to safely gain & use that new range of motion.
Additionally, anyone who spends a ton of time on their feet, jumps rope a ton (Practicing your double-unders like crazy?) or significantly increases their physical activity (from their normal baseline) could be at risk.
Since Plantar Fasciitis is basically a result of over-stressing the tissues of the foot and lower leg anyone who makes a significant change to the amount of stress they are placing on the feet and lower legs can run into issues.
How do I avoid Plantar Fasciitis (Or not make it worse)?
So now that we know that the primary cause of this all too common injury is over stressing the tissues of the lower leg and foot the best way to avoid it is to make sure you are not over-stressing those tissues!
Pretty simple huh?
But what does that really mean to me?
Basically, it depends on your current physical condition and previous training history but just about everyone can benefit from one simple thing:
Improve the mobility and flexibility of your feet, ankles, and calves.
If running less is not an option (because of mandatory PT or whatever) then the absolute most bang for you buck will come from spending a significant amount of time stretching and mobilizing.
While there are a million different stretches you could do I’m going to highlight my favorite below. Feel free to try them all and see what feels best for you.
Just remember, your body is a system of systems, so just because the bottom of your foot hurts doesn’t mean you should only focus on the bottom of your foot.
Anytime you’re dealing with a movement or mobility issue you should focus on the the stuff “above” and “below” the problem area as much, if not more, than the problem area itself.
So, like I mentioned above, if the bottom of your foot and/or heel is the problem, working on your calves, ankles, and toes can make a world of difference.
If you’ve been around Strategic Athlete for a while then you know that I’m ALL ABOUT getting the most bang for your buck when. it comes to any training, even if it’s recovery work.
Stretches to help your plantar fasciitis
Here are a few stretches you can do to improve your overall lower body mobility, as well as address that pesky plantar fasciitis.
The Standing Calf Stretch (Straight Leg & Bent Leg Variation)
With the straight leg variation you’ll feel more of a stretch in your upper calf and even the hamstring. With the foot “blocked” you’ll also be working on that ankle a bit.
In the bent leg variation you should feel that stretch “move” down into your achilles and heel.
Do both, spend at least 2:00 hitting each position on each leg.
The Cossack Squat
The cossack squat is one of my favorite lower body mobility movements and I include it in just about all of my warmups. If you focus on keeping your feet planted (not letting your heel come off the ground) you’ll get an awesome stretch from the feet all the way up to the hips.
Start off with 5-10 in each direction and try to hang out in the down position on each side for a few seconds each rep. As you gain mobility, spend a longer time in that down position.
The 10-Minute Squat Test
I love this one because I know how much it sucks and like to watch people suffer…
Well, that’s only part true because I also love this one because it will tell you exactly where you’re tight and need to spend more time. It’s also dead simple to do. Just squat ass to grass and hang out (totally passive).
Mobilizations to help your plantar fasciitis
Stretching is one thing, by self myofascial release is another tool you can use to get those soft tissues moving, sliding, and gliding like they’re supposed to.
Put simply, grab a lacrosse ball (or something similar) and mash your feet, ankles, and calves.
For more detailed info on this I’ll point you to someone WAY smarter than me:
Plantar Fasciitis – Dr. Kelly Starrett – Mobility WOD
Free Your Calcaneus- Dr. Kelly Starrett – Mobility WOD
Ultra Runner’s Feet
Mobility work is great, but how about strengthening the foot?
Ok, so you can use all those videos above to help fix plantar fasciitis that you already have as well as help prevent it from happening in the first place but mobility and flexibility is useless without the strength in that range of motion to go with it.
As you may have noticed in the first video above Kelly mentions that a ton of stress on the foot comes when the arch is allowed to collapse medially (towards your other foot – i.e. Flat Foot).
When this happens you put a ton of stress on the tissues in your foot and you are also over stretching the muscles of the lower leg in general. This pattern is a super common movement dysfunction, especially in folks who spend the majority of their days sitting (You know, like all of us).
When you spend the majority of your waking house in a seated position your glutes get “:turned off” and stuck/glued down and all kinds of stuff go wrong downstream.
This is something I addressed in our Shin Splints post.
That medial collapse of the foot and ankle, typically due to a lack of strength & stability in your glutes / external rotators, can also cause plantar fasciitis.
So if avoiding shin splints didn’t get you excited about squatting and lunging more, hopefully this will!
Best way to avoid this medial collapse?
Strengthen those glutes with stuff like squats, step-ups, hip thrusts, single leg deadlifts, and lunges.
If needed, take your shoes off and pay close attention to your feet during these exercises. Try your best to maintain an arch in your foot throughout the entire range of motion!
If that seems impossible then reduce the intensity (less weight, volume, more rest) and try again.
Personally, since most of my workout programming is heavily focused on building strong and durable hips, glutes, and legs I like to warm up and cool down with a few minutes of barefoot jump rope for a little extra conditioning of that foot, calf, and ankle complex as well.
Try this in your next warm-up:
5:00 of barefoot jump rope
The goal of this should be continuous movement. If you’re comfortable jumping rope then feel free to mix in single and double footed jumps, double-unders, and running in place.
I think you’ll notice that it is much harder than it sounds!
Wrapping it up
Unfortunately, some of the most common injuries attributed to running can be entirely prevented with smart training & smart recovery.
But this only happens by identifying the specific movement deficiency FIRST and then addressing the underlying problem, not just the symptoms (i.e. NSAIDs help with inflammation and can make your plantar fasciitis feel better but it’ll just come back if you don’t address the root cause!).
Which is why the term ""Movement Impairment Syndrome” is synonymous with the term ""musculoskeletal disorder”. If you can’t move correctly, you’re gonna end up with some sort of musculoskeletal disorder or injury!
All of those common remedies like ice, heat, and ibuprofen only serve to treat the symptoms and do absolutely nothing for the underlying cause of the problem.
You need to identify and correct the specific movement dysfunction first!
While plantar fasciitis can be super debilitating you should know that it can be fixed by allowing the inflammation to clear (rest, compression, movement, elevation will help) and then focusing on the root cause:
Your tissues are probably too weak, your mobility probably sucks, and you’re probably in a bad position.
A solid strength & conditioning program combined with some aggressive mobility work is likely all you need.
References
Sahrmann, S. A. (2002). Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis: Mosby.